Figure 2 From Risk Stratification Of Pleural Fluid Cytology Based On
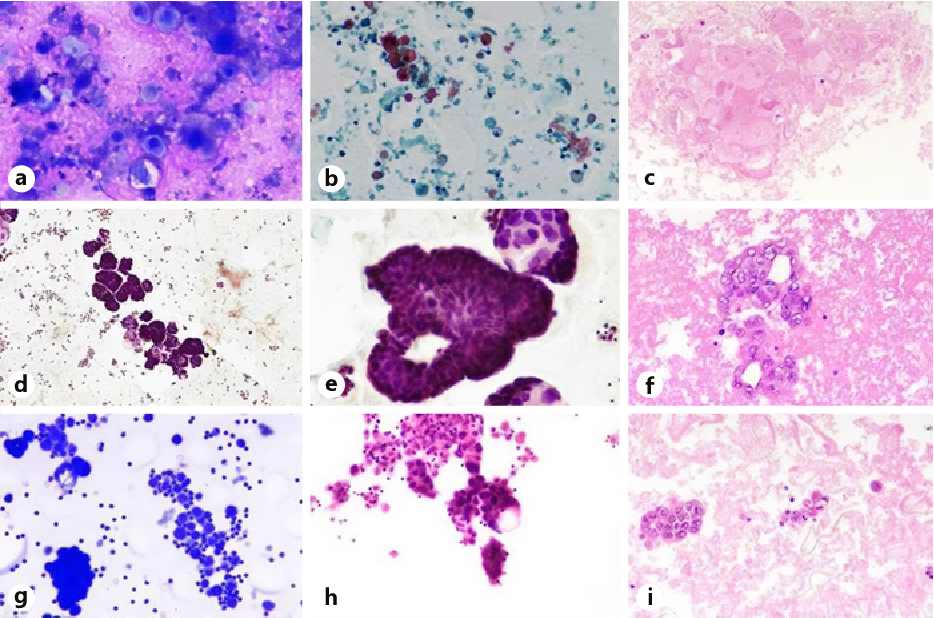
Figure 2 From Risk Stratification Of Pleural Fluid Cytology Based On The present study aims to reclassify pleural fluid cytology and calculate the risk of malignancy (rom) for each diagnostic category. material and methods: it is a retrospective 2 years observational study comprising 690 pleural fluid specimens. retrospective reviews were performed, and cases were reclassified into five categories as per tisrsfc. Fig. 2. a–f mal epithelial tumours, lung origin. a photomicrograph shows clusters and singly lying mal cells with squamoid cytoplasm in a necrotic background (mgg. ×400). b shows dyskeratotic squamous cells along with tumour diathesis in a dirty background (pap. ×100). c cell block shows a cluster of atypical squamous cells with the raised nucleo cytoplasmic ratio in a fibrino haemorrhagic.

Figure 2 From Risk Stratification Of Pleural Fluid Cytology Based On Risk stratification of pleural fluid cytology based on the international system for reporting serous fluid cytology in a tertiary care centre. Three characteristics were found, each of which was associated with over 70% of the exudates and, at most, one of the transudates: [1] a pleural fluid toserum protein ratio greater than 0.5; [2] a. The present study aims to reclassify pleural fluid cytology and calculate the risk of malignancy (rom) for each diagnostic category. <b><i>material and methods:< i>< b> it is a retrospective 2 years observational study comprising 690 pleural fluid specimens. A systematic approach to analysis of the fluid assists clinicians in narrowing the differential diagnosis or establishing the cause of an effusion. in addition to its diagnostic value, pleural fluid analysis also has predictive value (ie, estimates of the likelihood of a clinical response to pleural fluid drainage) and prognostic value (eg.

Figure 2 From Risk Stratification Of Pleural Fluid Cytology Based On The present study aims to reclassify pleural fluid cytology and calculate the risk of malignancy (rom) for each diagnostic category. <b><i>material and methods:< i>< b> it is a retrospective 2 years observational study comprising 690 pleural fluid specimens. A systematic approach to analysis of the fluid assists clinicians in narrowing the differential diagnosis or establishing the cause of an effusion. in addition to its diagnostic value, pleural fluid analysis also has predictive value (ie, estimates of the likelihood of a clinical response to pleural fluid drainage) and prognostic value (eg. The present study estimates the sensitivity of pleural fluid cytology in patients with confirmed pleural malignancy and evaluates whether clinical and fluid characteristics might help clinicians identify patients at risk of false negative cytology results. for all patients with mpe, pleural fluid cytology had a sensitivity of 75.0%. The foundation of the further diagnostic work‐up is the thoracocentesis (pleural tap) which enables the differentiation of a transudate from an exudate. 2 a standard panel of tests includes pleural fluid protein, glucose, ph, lactate dehydrogenase (ldh), cytology, and microbiology. 2 table 1 shows the differential diagnosis of pleural fluids.

Table 2 From Risk Stratification Of Pleural Fluid Cytology Based On The The present study estimates the sensitivity of pleural fluid cytology in patients with confirmed pleural malignancy and evaluates whether clinical and fluid characteristics might help clinicians identify patients at risk of false negative cytology results. for all patients with mpe, pleural fluid cytology had a sensitivity of 75.0%. The foundation of the further diagnostic work‐up is the thoracocentesis (pleural tap) which enables the differentiation of a transudate from an exudate. 2 a standard panel of tests includes pleural fluid protein, glucose, ph, lactate dehydrogenase (ldh), cytology, and microbiology. 2 table 1 shows the differential diagnosis of pleural fluids.

Comments are closed.